Balancing Your Vaginal Microbiome: A Functional Nutritionist's Approach to Health and Comfort
As a functional nutritionist, I consistently see how imbalances in the vaginal microbiome, known as dysbiosis, can lead to persistent discomfort and recurrent infections. Beyond the immediate irritation of bacterial vaginosis (BV) and yeast infections, dysbiosis can significantly heighten the risk of urinary tract infections (UTIs) and subtly impact hormone and bladder health. The good news? A targeted, holistic approach rooted in functional nutrition and lifestyle medicine offers a powerful pathway to restore harmony and foster lasting comfort and well-being. This isn't just about managing symptoms; it's about building resilience.
The Vaginal Microbiome and Dysbiosis: An Ecosystem in Focus
Understanding the delicate ecosystem of the vaginal microbiome is foundational to achieving optimal health.
Let's explore why balance is so important and what happens when things go awry.
The Crucial Role of a Balanced Microbiome
Imagine your vaginal microbiome as a thriving, well-tended garden. In this healthy state, beneficial Lactobacillus species flourish, acting as the diligent gardeners. These beneficial bacteria produce lactic acid, which is essential for maintaining a normal acidic vaginal pH (typically 3.8-4.5). This acidity is your body's natural defence, creating an inhospitable environment for pathogenic microorganisms. Furthermore, a balanced microbiome actively produces antimicrobial compounds, offering an additional layer of protection against infections. It is this intricate balance that promotes comfort and prevents disease.
Understanding Dysbiosis and Its Systemic Effects
Dysbiosis occurs when this finely tuned ecosystem is disrupted, much like weeds overwhelming our carefully cultivated garden. This shift sees a reduction in protective Lactobacillus and an overgrowth of opportunistic bacteria or yeast. This can manifest as bacterial vaginosis, characterised by an elevated pH and malodour, or recurrent yeast infections.
Critically, the impact of dysbiosis extends beyond the vagina. It can significantly increase susceptibility to urinary tract infections and influence overall pelvic health. This ripple effect underscores the importance of a comprehensive approach to maintaining microbial balance.
Recognising the Signals of an Imbalanced Microbiome
Being attuned to your body's signals is paramount. Common indicators of dysbiosis include unusual discharge (changes in colour, consistency, or volume), persistent odour, itching, burning, or discomfort during intercourse or urination. These symptoms can fluctuate, appearing intensely at times and receding at others. It's also important to remember that not all imbalances present with overt symptoms immediately. Regular self-awareness, combined with professional guidance when necessary, can help identify and address issues early.
Natural Approaches to Rebalance and Restore
Restoring balance to your vaginal microbiome involves supporting its inherent protective mechanisms.
Functional nutrition and specific interventions provide powerful tools for this.
Targeted Probiotics: Reinforcing Your Defences
From a functional perspective, not all probiotics are created equal, especially when it comes to vaginal health. We look for specific, well-researched Lactobacillus strains known for their efficacy in the vaginal environment:
Lactobacillus crispatus
Lactobacillus jensenii
Lactobacillus gasseri
Lactobacillus rhamnosus
Lactobacillus reuteri
These strains are chosen for their ability to:
Lower vaginal pH by producing lactic acid, thereby re-establishing the crucial acidic protective barrier.
Produce hydrogen peroxide, which directly inhibits the growth of harmful bacteria.
Restore Lactobacillus dominance, particularly critical after antibiotic use, which can indiscriminately reduce beneficial bacteria.
Significantly reduce the recurrence of BV and yeast infections.
You can find these targeted strains in high-quality oral probiotic supplements. For a more direct approach, specific vaginal probiotic suppositories are also available. For access to practitioner-only probiotic recommendations, feel free to email me at info@testwisenutrition.com.au.
📌 Evidence-Based Support: A double-blind, placebo-controlled trial by Laue et al. (2018) demonstrated significant improvements in BV outcomes using specific Lactobacillus strains.
Lactulose Tampon Therapy: A Prebiotic Strategy (Short-Term & Guided Use)
Lactulose tampon therapy is a fascinating, lesser-known approach that leverages the power of prebiotics. Lactulose, a non-absorbable sugar, acts as a selective food source for beneficial Lactobacillus species. When applied locally, it can stimulate the growth of these beneficial bacteria, boosting lactic acid production and helping to normalise vaginal pH.
How it generally works: This involves soaking a tampon in a diluted lactulose solution and inserting it for approximately one hour daily during acute symptom flares or as a short-term intervention after antibiotic use.
Critical Note: This therapy should always be undertaken with professional guidance to ensure proper preparation, safe application, and suitability for your individual circumstances.
Addressing Related Conditions: UTI Prevention and Hormonal Influences
The interplay between vaginal, bladder, and hormonal health is profound.
A holistic approach considers all these factors.
Nutritional Strategies for UTI Prevention
Recurrent UTIs are often linked to vaginal dysbiosis. Specific nutritional support can bolster your defences:
D-Mannose: This simple sugar helps prevent bacteria, particularly E. coli, from adhering to the walls of the urinary tract. Instead, these pathogens are naturally flushed out through urination.
Cranberry Extract: Rich in proanthocyanidins (PACs), cranberry compounds also interfere with bacterial adhesion to the urinary tract lining.
Probiotics: As discussed, a healthy vaginal microbiome acts as a barrier, reducing the translocation of bacteria from the vaginal area to the urethra, thus playing a key role in UTI prevention. You can find vaginal health probiotics here.
Hydration: Consuming adequate water (aim for ~2.7 litres daily, adjusting for activity and climate) is crucial for flushing the urinary system.
Effective UTI Prevention Strategies Beyond Supplements
Simple lifestyle habits significantly reduce UTI risk:
Proper Wiping Technique: Always wipe from front to back after using the toilet to prevent bacteria from entering the urethra.
Urination Habits: Urinate before and immediately after sexual activity to help flush out any bacteria introduced during intercourse.
Breathable Underwear: Opt for cotton underwear and avoid prolonged wearing of tight-fitting clothing to reduce moisture and allow airflow, which discourages bacterial growth.
Avoid Irritants: Strictly steer clear of harsh soaps, douches, and scented feminine hygiene products that can disrupt the delicate vaginal pH.
Hormonal Influences on Vaginal Health
Estrogen is a key hormone for vaginal health. It maintains the thickness, elasticity, and overall health of vaginal tissues, and supports the production of glycogen, which feeds Lactobacillus and sustains an acidic pH.
During periods of fluctuating or declining estrogen, such as perimenopause, menopause, or certain hormonal birth control regimens, women may experience:
Increased vaginal pH: Making the environment more hospitable for pathogens.
Reduced Lactobacillus populations.
Vaginal atrophy: Thinning and weakening of vaginal tissues, leading to dryness and increased susceptibility to irritation and infection.
If hormonal shifts are contributing to your vaginal health concerns, discussing this with a healthcare provider is essential. They may explore options such as local estrogen therapy to restore tissue health and pH balance.
Comprehensive Nutritional and Lifestyle Support
Your daily nutrition and lifestyle habits are the foundation of lasting vaginal health.
Building on this foundation with targeted interventions can help support optimal wellbeing.
Key Nutrients and Botanicals for Vaginal Health:
Vitamin D: Low levels are correlated with an increased risk of BV (up to 4.3 times higher) and are crucial for robust immune function and antimicrobial defences.
Vitamin C: Essential for collagen formation and maintaining the integrity of mucosal tissues (consider 500–2,000 mg twice daily, as tolerated).
Green Tea Extract: Provides potent antioxidant and broad-spectrum antimicrobial properties.
Sea Buckthorn Oil: Rich in omega-7 fatty acids, this botanical is excellent for supporting the repair, hydration, and overall health of mucosal membranes throughout the body, including the vagina.
Pumpkin Seeds: These nutrient-dense seeds contain cucurbitacin, an amino acid that has shown antiparasitic properties. They are also a good source of zinc, which is crucial for immune function and tissue repair, both of which are vital for maintaining vaginal health. Read more on the benefits of pumpkin seeds.
Aloe Vera: Known for its soothing and anti-inflammatory properties, oral aloe vera can support gut health, which has downstream effects on the vaginal microbiome. Topical, high-quality, pure aloe vera gel (always perform a patch test first) may also provide soothing relief for external irritation. Explore research on aloe vera's benefits.
Dietary Strategies for a Thriving Microbiome:
Prebiotic-Rich Foods: Incorporate garlic, onions, leeks, asparagus, and bananas into your diet. These fermentable fibres selectively nourish beneficial Lactobacillus species, promoting a balanced microbiome.
Omega-3 Fatty Acids: Found in fatty fish (salmon, mackerel), flaxseeds, chia seeds, and walnuts, omega-3s are powerful anti-inflammatory agents that support healthy vaginal tissue and may help alleviate dryness.
Herbal Support: Certain herbs, used mindfully, can complement your strategy. Examples include calendula (known for soothing tissues), echinacea (for immune support), and goldenseal (for its antimicrobial properties). Always consult a qualified professional before incorporating herbal remedies.
Limit Refined Sugars and Processed Carbohydrates: These foods can fuel the overgrowth of pathogenic yeast and bacteria, sabotaging your efforts to achieve balance.
Hydration: Maintain optimal hydration (aim for ~2.7 litres of filtered water daily) and include water-rich foods like cucumbers, celery, and oranges to support natural lubrication and systemic health.
Minimise Endocrine Disruptors: Be mindful of chemicals found in scented feminine hygiene products, certain plastics (BPA/BPS), and pesticides. Opt for unscented, natural products and organic foods whenever possible to minimise exposure to compounds that can disrupt hormonal balance.
Empowering Lifestyle Habits:
Stress Management: Chronic stress can negatively impact your immune system and overall microbial balance. Incorporate practices such as mindfulness, yoga, meditation, or spending time in nature to help mitigate stress.
Avoid Irritants: Strictly avoid douching, harsh, chemical-laden soaps, and scented feminine hygiene products, which strip away protective natural oils and disrupt the pH balance.
Breathable Clothing: Opt for natural, breathable fabrics like cotton for underwear and avoid wearing tight-fitting garments that trap moisture and heat for prolonged periods.
Safe Sex Practices: Practice safe sex, and in cases of recurrent BV, consider whether partner treatment may be appropriate, as it can sometimes be a factor in re-infection.
How a Functional Nutritionist Can Help: Going Deeper
As a functional nutritionist, my role is to empower you with personalised strategies by looking at your health holistically.
We don't just treat symptoms; we identify and address the root causes of imbalances.
Advanced Functional Testing:
A key aspect of functional nutrition is leveraging advanced testing that goes beyond conventional diagnostics to provide a nuanced picture of your internal environment.
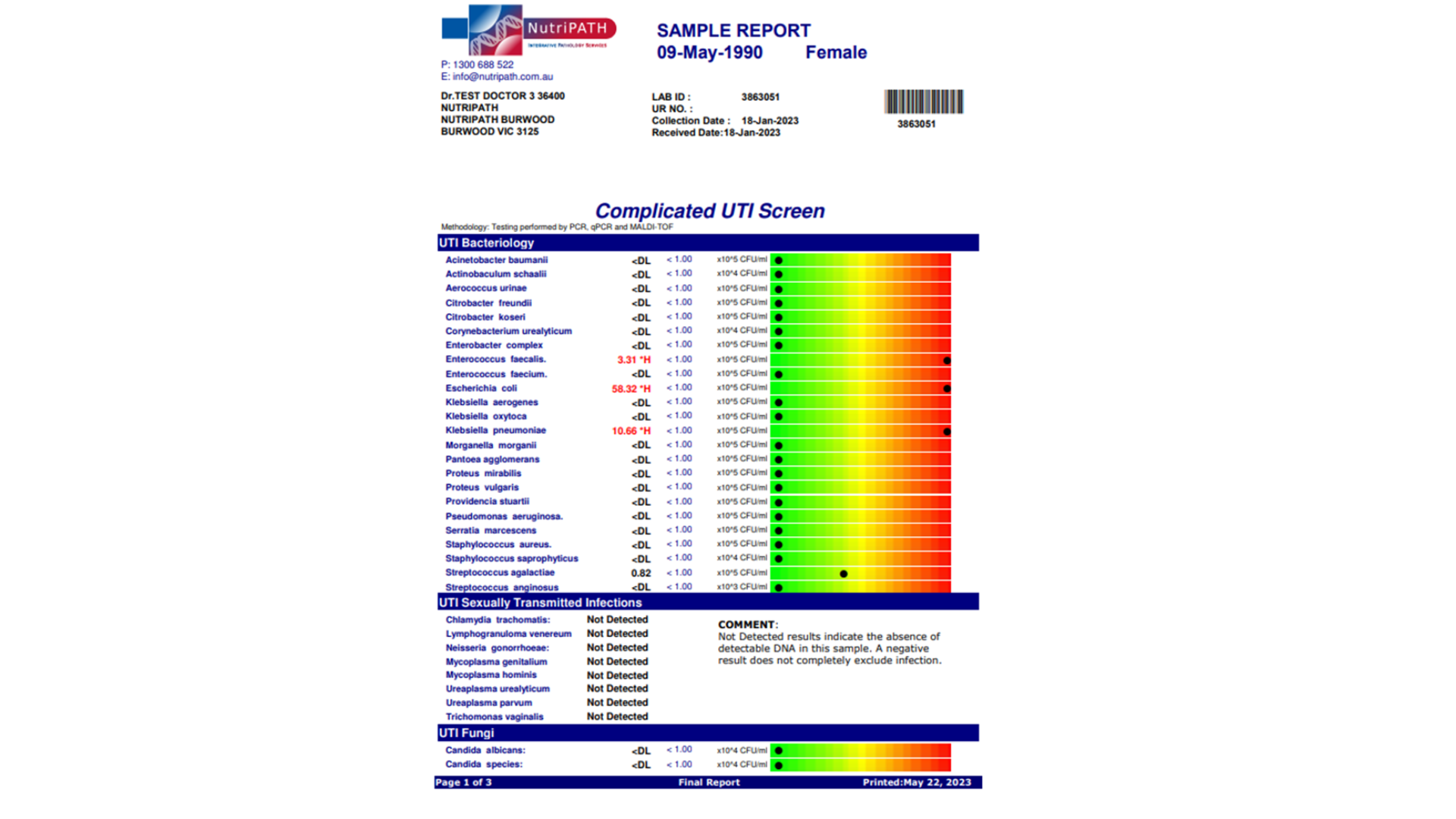
Nutripath Vaginal Microbiome Testing: This specialised test can provide a detailed map of the bacterial and fungal species present in your vaginal microbiome. This granular data allows for highly targeted probiotic, prebiotic, and dietary interventions, moving beyond guesswork.
Comprehensive UTI Testing: For recurrent UTIs, we can explore advanced urine testing that may detect a broader spectrum of bacterial strains, including those that might evade standard culture methods, enabling more effective treatment strategies.
For more information on advanced testing methods, check out this recent study.
The Takeaway: A Holistic Path to Lasting Vaginal Health
Optimising vaginal health is an integral part of overall well-being. It's not merely about eradicating infections; it's about fostering resilience within your microbiome, supporting healthy hormone balance, and nourishing your tissues from the inside out.
By integrating targeted probiotics, personalised nutrition, mindful lifestyle habits, and, when indicated, medical support, you can significantly reduce the recurrence of BV, yeast infections, and UTIs, while dramatically improving comfort, confidence, and your overall quality of life.
Michelle Hislop,
TestWise Clinical Nutritionist
👉 Take control of your vaginal health today.
Book a consultation to explore targeted probiotics, nutritional strategies, lifestyle changes, and professional support tailored to your needs.
Disclaimer:
The information in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. It should not replace consultation with a qualified healthcare professional who can assess your individual health needs. Always seek the guidance of your doctor or other qualified health provider before starting, changing, or discontinuing any medication, supplement, or treatment.