Curious About Your Gut Health? Learn How a Whole Food Diet Can Make a Difference
As Natural Practitioners we often jump straight to supplements when looking at microbiome test results!
But sometimes the most powerful tool is food!
Curious about what your gut might be trying to tell you? You're not alone. More and more people are realising how strongly diet shapes gut health, especially when it comes to calming inflammation and easing digestive discomfort.
In this post, I want to share the story of a 48-year-old traveller whose stool analysis revealed high levels of pathobionts, including Escherichia coli and Clostridium perfringens, as well as inflammation markers such as hexa-LPS. Instead of reaching for a long list of supplements, this client, with my help, focused on a whole food dietary shift—and the results were transformative.
If you’re navigating gut symptoms or want to support your microbiome diversity, this example serves as a reminder that sometimes the biggest changes can start right on your plate.
The Role of Pathobionts
Pathobionts are microorganisms that typically exist harmlessly in our gut but can become problematic under certain conditions. These organisms play a complex role in our digestive health.
When our gut environment is balanced, pathobionts coexist peacefully with beneficial bacteria. However, factors such as stress, a poor diet, or the use of antibiotics can disrupt this balance.
In an unbalanced state, pathobionts may multiply rapidly, leading to various digestive issues. This overgrowth can cause inflammation, discomfort, and even contribute to more serious health problems.
Understanding the role of pathobionts is crucial for maintaining optimal gut health. By keeping these microorganisms in check, we can support a healthier digestive system overall.
Key Players: Clostridium Perfringens and Others
Clostridium perfringens is one of several key players in the complex ecosystem of our gut microbiome. This bacterium, along with others, can significantly impact our digestive health.
C. perfringens is commonly found in small amounts in healthy individuals. However, when it overgrows, it can lead to symptoms similar to food poisoning and other gastrointestinal issues.
Other important microbes include Escherichia coli and various species of Lactobacillus and Bifidobacterium. Each plays a unique role in maintaining gut health or, conversely, contributing to digestive problems when out of balance.
Understanding these key players helps us better manage our gut health. By fostering a balanced microbiome, we can support better overall health and well-being.
Systemic Inflammation and Hexa-LPS
Systemic inflammation and hexa-LPS (lipopolysaccharides) are closely linked to gut health and can have far-reaching effects on our bodies.
Let's explore their relationship and impact.
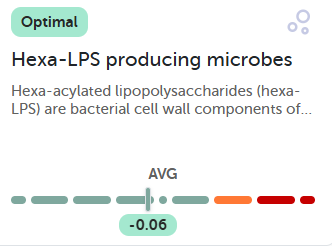
Hexa-LPS are components of certain bacteria's cell walls. When these bacteria overgrow or die, they release hexa-LPS, which can trigger an immune response and inflammation.
This inflammation isn't limited to the gut. It can become systemic, affecting various parts of the body and potentially contributing to chronic health issues.
High levels of hexa-LPS-producing microbes in the gut can indicate an imbalance in gut microbiota. This imbalance may lead to increased intestinal permeability, often referred to as "leaky gut," further exacerbating systemic inflammation.
Understanding the connection between gut health, hexa-LPS, and systemic inflammation underscores the importance of maintaining a balanced microbiome for overall health.
Dietary Interventions for Improved Digestive Health
Diet plays a pivotal role in shaping our gut health. Let's explore how dietary changes can positively impact our digestive system and overall well-being.
Transitioning to a Whole Food Diet
“If it didn’t grow in the ground or have a pulse, it probably doesn’t belong on your plate.”
Transitioning to a whole food diet can significantly improve gut health and overall well-being. This dietary approach focuses on consuming foods in their natural, unprocessed state.
Whole foods are rich in fibre, which feeds beneficial gut bacteria and promotes regular bowel movements. They also contain a wide range of nutrients that support overall health.
Making this transition involves gradually replacing processed foods with whole alternatives. Start by incorporating more whole fruits, vegetables, gluten-free whole grains, and lean proteins into your meals.
It's essential to make changes slowly to allow your body to adjust. This gradual approach can help minimise digestive discomfort and make the transition more sustainable.
Remember, everyone's dietary needs are unique. Consulting with a healthcare professional can help you create a personalised plan that works best for you.
The Impact of Dietary Changes on Microbiome Diversity
Dietary changes can have a profound impact on the diversity of our gut microbiome. A varied diet rich in whole foods supports a more diverse and resilient microbial community.
Increasing dietary diversity introduces a wider range of nutrients and compounds that different beneficial bacteria can thrive on. This, in turn, promotes a more balanced and robust microbiome.
A diverse microbiome is better equipped to handle potential disruptions and maintain overall gut health. It can also contribute to improved digestion, nutrient absorption, and immune function.
Conversely, a diet high in processed foods and low in variety can lead to a less diverse microbiome. This can make the gut more susceptible to imbalances and potential health issues.
By consciously choosing a variety of whole foods, we can actively support and enhance the diversity of our gut microbiome.
Addressing Intestinal Inflammation through Diet
Diet plays a crucial role in managing intestinal inflammation.
Certain foods can either exacerbate or alleviate gut inflammation.
Anti-inflammatory foods, such as fatty fish, spices like turmeric, leafy greens, and berries, can help reduce gut inflammation. These foods are rich in omega-3 fatty acids, antioxidants, and other beneficial compounds.
On the other hand, processed foods, refined sugars, and certain oils can promote inflammation. Reducing or eliminating these from your diet can help manage intestinal inflammation.
Incorporating fermented foods, such as yogurt, kefir, and sauerkraut, can also be beneficial. These foods contain probiotics that support gut health and may help reduce inflammation.
Remember, individual responses to foods can vary. It's essential to pay attention to how your body reacts and adjust your diet accordingly.
Case Study: A 48-Year-Old's Diet Transition
Let's explore a real-life example of how dietary changes can impact gut health, focusing on the journey of a 48-year-old individual.
Initial Gut Health Challenges
Our case study subject, a 48-year-old frequent traveller, faced some gut health challenges. These issues stemmed from multiple bouts of gastroenteritis contracted during overseas trips.
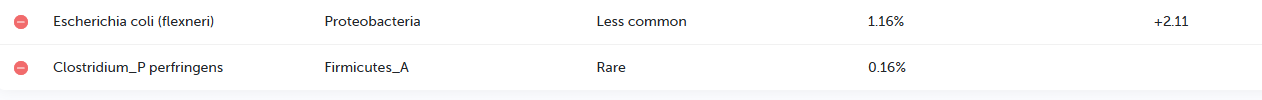
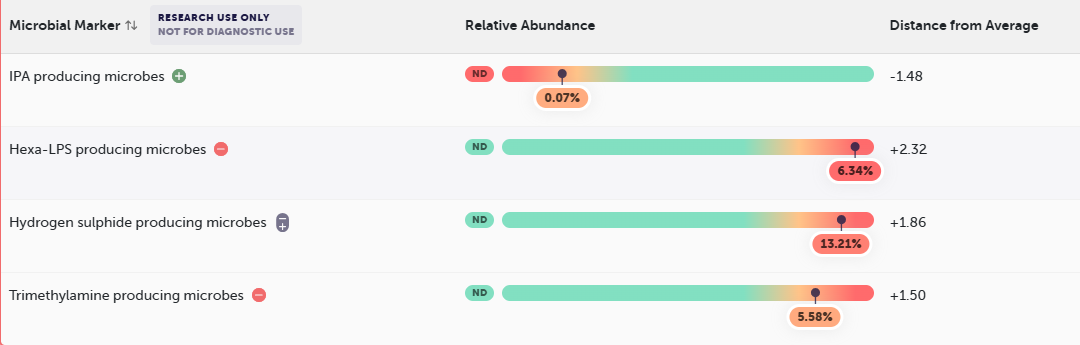
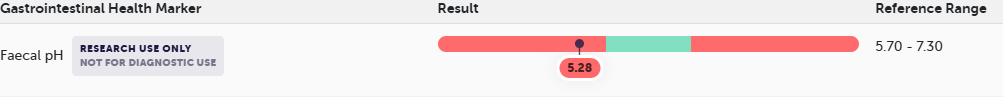
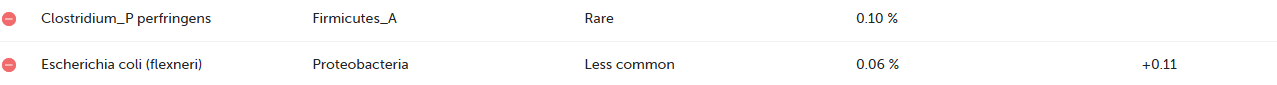
Initial Comprehensive Stool Test revealed several concerning factors:
High levels of pathobionts, including Escherichia coli and Clostridium perfringens.
Elevated markers of systemic inflammation, particularly hexa-LPS
Low pH in the stool, indicating a rapid transit time
These results suggested a dysbiosis in the gut microbiome, potentially contributing to ongoing digestive issues and discomfort.
The individual reported feeling that their gut was "not normal," highlighting the impact these imbalances can have on overall well-being.
Results of the Whole Food Diet Transition
From processed-heavy to whole-food strong—this client made the shift, and their gut thanked them.
Following the initial assessment, with my guidance, the individual embarked on a significant dietary transition. They transitioned from a typical “Western diet” high in processed foods to a whole-food-based approach.
Key changes in the new diet included:
Increased the variety of fruits and vegetables, to help increase his antioxidant and polyphenol content.
Focused on adding gluten-free whole grains
Focus on healthy protein sources, including increasing his intake of oily fish.
Added nuts, seeds, legumes, and beans.
Significant reduction in gluten, dairy, and alcohol consumption
For further insights and dietary tips, visit the blog page on Helping Your Family Build a Healthy Microbiome!
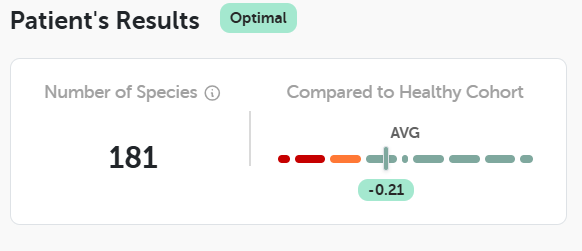
After several months on this new dietary regimen, follow-up testing revealed remarkable improvements:
“No gastrointestinal health markers were out of range, including the client’s PH”.
Microbiome diversity increased from 164 to 181 species.
LPS levels dropped dramatically from 6.34% to -0.06%.
Clostridium_P perfringens had decreased from 0.16% to 0.10%.
Escherichia coli from 1.16% to 0.06%.
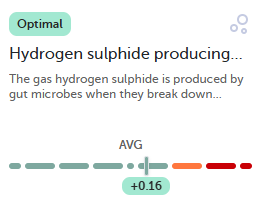
Hydrogen Sulphide producing bacterias 13.21% to 0.16%.
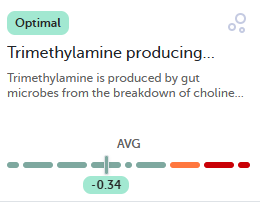
Trimethylamine producing microbiomes 5.58% to -0.34%.
These results demonstrate the significant impact of dietary changes on improving gut health and altering microbiome composition.
Encouraging Outcomes and Next Steps
The outcomes from this dietary transition are inspiring and highlight how nutrition can play a central role in restoring gut balance.
Key takeaways from this case study:
A noticeable increase in microbiome diversity
A dramatic reduction in inflammation markers
The normalisation of several gut health parameters
Together, these changes point to a more balanced, resilient gut ecosystem—one that supports better overall health and well-being.
How a Nutritionist Can Help
This case study shows that targeted dietary changes, guided by a nutrition professional, can make a real difference. Instead of leaning heavily on supplements, the focus here was on food-first strategies that calmed inflammation and helped rebalance the microbiome.
With personalised support, a nutritionist can:
Review your current diet and identify areas for improvement
Recommend probiotic-rich foods and prebiotics to feed beneficial bacteria
Create a practical, gut-friendly meal plan tailored to your lifestyle
Interpret stool test results and translate them into clear, actionable steps
Guide you through reintroducing foods and adjusting your diet as your gut heals
Having this kind of professional guidance takes out the guesswork and helps you move forward with confidence, making your gut health journey smoother, more sustainable, and more effective.
Explore Further
For family-friendly nutrition tips and free recipes, explore the Well Nourished membership page.
For more details on microbiome testing, visit our gut testing information page.
Remember, every gut health journey is unique. Be patient with your body as it restores balance, and reach out for professional support if you need it.
Michelle Hislop, TestWise Clinical Nutritionist
Book a consultation to explore stool testing for yourself.
Disclaimer:
The information in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. It should not replace consultation with a qualified healthcare professional who can assess your individual health needs. Always seek the guidance of your doctor or other qualified health provider before starting, changing, or discontinuing any medication, supplement, or treatment.