Why Some UTIs Don’t Go Away – And How Advanced Testing Can Help
“Recurring UTIs? It might not be ‘all in your head.’
Discover how your vaginal microbiome could be the key.
A client came to me after six months of constant UTI symptoms. She had tried multiple rounds of antibiotics, but the discomfort always returned. Standard GP tests continued to show “no infection,” leaving her without answers.
Sounding familiar?!
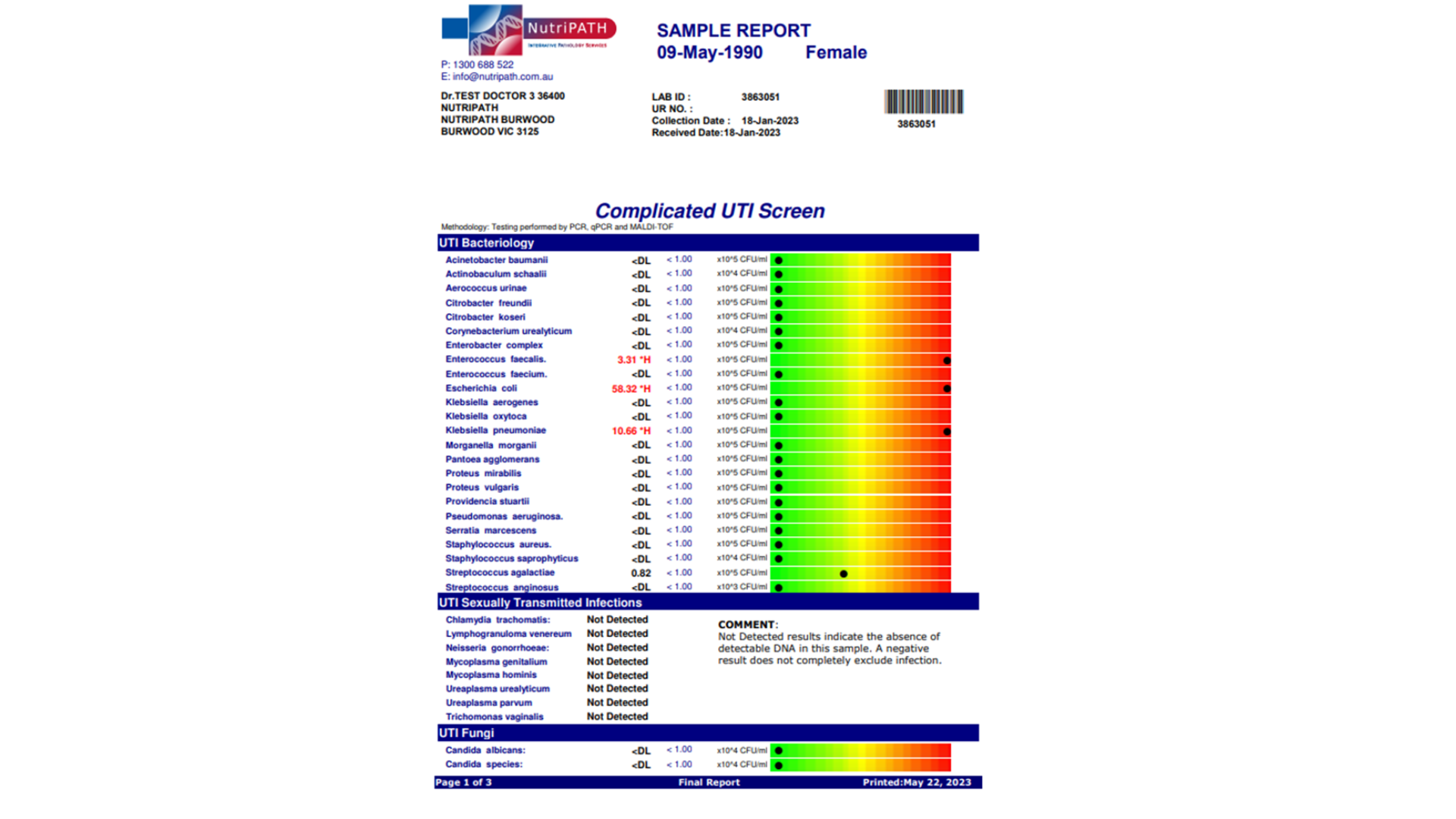
She then completed the Nutripath Complicated UTI and Vaginal Microbiome Profile Panels.
Her results showed:
High levels of opportunistic bacteria: Enterococcus faecalis
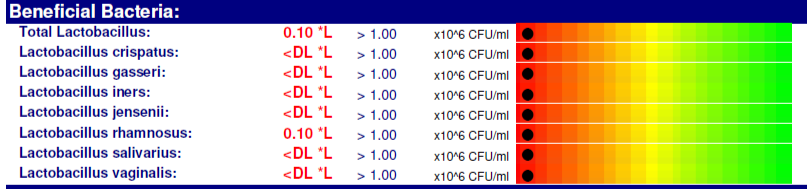
Very low levels of “protective” vaginal Lactobacillus bacteria (including L. crispatus, L. gasseri, L. iners, L. jensenii, and others.
Vaginal pH of 4.5: at the upper end of normal and bordering on alkaline. A healthy range is typically between 3.5 and 4.5, and even slight increases can make the environment more hospitable to unwanted bacteria.
“Without enough good bacteria, her vaginal microbiome was left vulnerable — and the results showed it.”
This explained why her symptoms wouldn’t resolve. With hardly any protective bacteria, an overgrowth of less friendly microbes, and a less acidic pH, her urinary tract environment was unbalanced and vulnerable.
What This Means for Recovery
The results gave us a clear direction for her care. Instead of another round of antibiotics, the focus shifted to:
Restoring protective bacteria
Using specific probiotics and lifestyle support to bring back beneficial Lactobacillus species that protect the urinary and vaginal microbiome.
Reducing opportunistic bacteria
Supporting her body with gentle, natural therapies to rebalance the microbial environment.
Balancing pH levels
Encouraging a healthier, more acidic vaginal environment that naturally discourages the growth of opportunistic bacteria.
Checking hormone health
Because estrogen levels often decline during perimenopause, which can reduce Lactobacillus populations and change the vaginal environment, it’s important to review hormone balance as part of a long-term plan.
Preventing future recurrence
With a stronger, more balanced microbiome, her risk of recurring UTIs could be reduced in the long term.
The Takeaway
If you’ve been struggling with UTIs that keep coming back, or symptoms that never fully clear despite antibiotics, it may not be “just in your head.” Standard urine tests often fail to detect hidden imbalances. As a certified clinical nutritionist who specialises in complex functional testing, tools like the Nutripath Complicated UTI Screening and Vaginal Microbiome assessment can help uncover the real reasons behind persistent symptoms and guide a more personalised path to recovery.
For more tips on how you might like to visit my blog on “Lifestyle Solutions for Optimising Vaginal Health”.
👉 Ready to get answers? Book a consultation today to see if this test could be right for you.
Michelle Hislop, TestWise Clinical Nutritionist
Disclaimer:
The information in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. It should not replace consultation with a qualified healthcare professional who can assess your individual health needs. Always seek the guidance of your doctor or other qualified health provider before starting, changing, or discontinuing any medication, supplement, or treatment.